Among all pathological processes that affect the spine in its various parts, cervical osteochondrosis is considered one of the most common. This disease leads to many complications, mainly because it affects the spinal cord and also negatively affects the functioning of the brain.
According to statistics for 2017, the disease has become significantly younger. If previously osteochondrosis mainly affected people after the age of 40, today various stages of cervical osteochondrosis are diagnosed in 90% of people over 25 years old. For this reason, it is important to know as much as possible about the pathology, from what it is to treatment methods.

What is cervical osteochondrosis?
In medical practice, the words cervical osteochondrosis mean an acquired progressive disease that affects a certain part of the spine. This pathological process is characterized by degenerative-dystrophic processes in the tissues of the intervertebral discs, which are shock absorbers for the cervical vertebrae.
Degenerative-dystrophic changes in the intervertebral discs are caused by the fact that they are worn and deformed. As a result, the distance between the vertebrae decreases and as a result the following consequences occur:
- Narrowing of the spinal canal in certain areas of the spine.
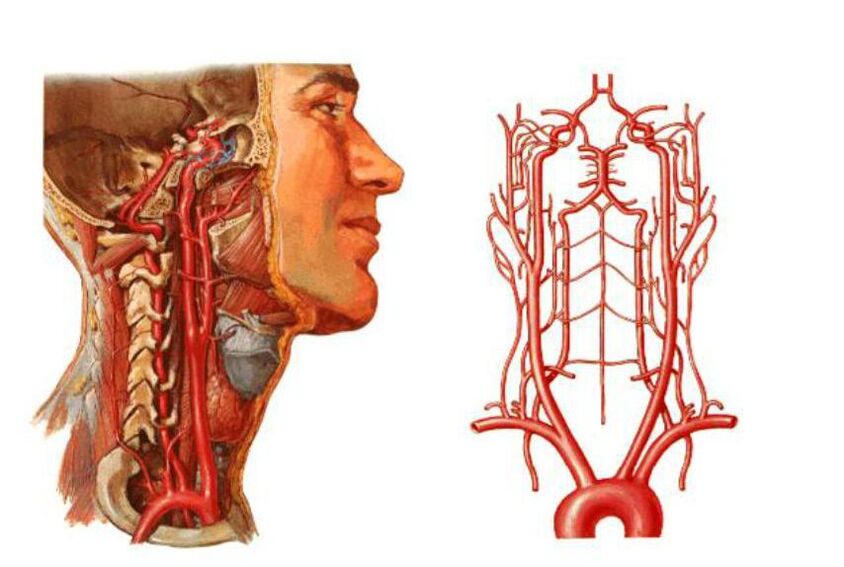
- Compression of the vertebral arteries - the large blood vessels that supply blood to the brain. Because of this, the supply to the brain deteriorates and blood circulation in the cervical spinal cord is interrupted.
- Intervertebral discs can be deformed and flattened. This leads to compression of certain areas of the spinal cord and nerves, most commonly nerve root compression.
All these problems threaten not only damaged blood circulation in the brain, neck pain, headaches, etc. The development of osteochondrosis of the cervical spine is dangerous with neurological problems, deterioration of the central nervous system and damage to brain tissue.
According to the international classification of diseases, osteochondrosis of the cervical spine is assigned several special codes. The disease code according to ICD 10 depends on the age at which the disease was diagnosed:
- M02 – intervertebral disc dystrophy in adolescence.
- M42. 12 – degenerative process in the neck area in adults.
Many factors depend on the age of the patient and the degree of development of the pathological process, for example, the consequences, complications, symptoms and, of course, the principles of treatment.
Causes
Knowing the causes of the development of cervical osteochondrosis can play a decisive role in the diagnostic process, as well as in determining the principles of combating the disease.
However, before listing the reasons, it is worth saying that doctors identify two factors that lead to the development of this pathological process:
- Pathological - the destruction of intervertebral discs and other vertebral structures with the involvement of nearby tissues, vessels and nerve bundles in the pathological process occurs under the influence of adverse external factors. The more severe these factors and other pathologies are, the faster the disease develops.
- Physiological - the development of pathology is mainly based on age-related changes. It is about the natural aging of cartilage tissue in the spine, salt deposits, etc.
If we list the most specific causes of cervical osteochondrosis, they are as follows:
- Disorders of metabolic processes in the body, as well as certain stages of obesity.
- Physical inactivity is a phenomenon characterized by limited mobility. We're not just talking about injuries or illnesses, this includes a sedentary lifestyle and sedentary work.
- Pathologies of the cardiovascular system that contribute to impaired blood circulation in the brain, pressure changes, etc.
- Bad posture includes various forms of scoliosis, rheumatism and even flat feet.
- Cervical spine injury. In this case it is about sprains, blows, bruises. Injuries to other parts of the spine can affect the development of cervical osteochondrosis.
- Excessive physical stress on the cervical spine, caused by intense sports or severe physical difficulties, depending on the type of activity of the person.
- A sedentary lifestyle is also dangerous because of the constant tension on the cervical spine and the entire spine if you sit incorrectly or on uncomfortable furniture.
- Hernia of the cervical spine, as well as various associated diseases.
- Forced holding of the head for a long time in an uncomfortable or unnatural position. In this case, not only muscle tension occurs, but also the spine in the cervical region is bent.
- Doctors consider constant stress and nervous tension as a very common cause.
- Congenital anomalies in the structure of the spine are also considered one of the reasons.

What health risks does it pose?
As mentioned earlier, the cervical spine region contains not only the spinal cord and various nerve branches, but also the vertebral arteries that supply blood to the occipital part of the brain, cerebellum and medulla oblongata.
With the development of cervical osteochondrosis, nearby tissues become inflamed. In addition, the development of pathology threatens to compress nerve roots and squeeze blood vessels, the consequences of which are as follows:
- Osteochondrosis is associated with deformations of the spine, resulting in the narrowing of the spinal canal in certain areas. This can lead to compression of the spinal cord and nerve branches, which promises severe neurological problems. In severe cases, a person feels pain, and there is even a possibility of losing control over certain parts of the body (mainly in the arms or face).
- Compression of the vessels of the neck, as already mentioned, is associated with impaired circulation in the occipital region of the brain. In this case, the brain stops receiving oxygen and nutrients in the necessary quantities and oxygen starvation begins. If blood circulation is impaired, there is a real risk of ischemic stroke and various neurological pathologies.
syndromes
Speaking of the danger posed by cervical osteochondrosis, as it progresses and lacks proper treatment, the disease can lead to a number of complications and syndromes.
The main syndromes are:
- Vertebral.
- Vertebral artery.
- Koreshkovy.
- Cardiac.
It is important to know that each of these symptoms is accompanied by painful sensations of a different nature, as well as a host of unfavorable clinical signs. A person may feel dizzy, tinnitus and much more.
Vertebral syndrome
It speaks of a direct connection between cervical osteochondrosis and bone and cartilage tissue. The symptoms of this type of pathology are also associated with damage to the mentioned tissues:
- Neck movements are partially or completely restricted.
- Head movements are accompanied by painful sensations in the neck area.
- X-rays show morphological changes in tissues (intervertebral and vertebral bodies).
It is worth noting that vertebral syndrome is always associated with these three clinical signs. If at least 1 of them is missing, the diagnosis will be completely different.
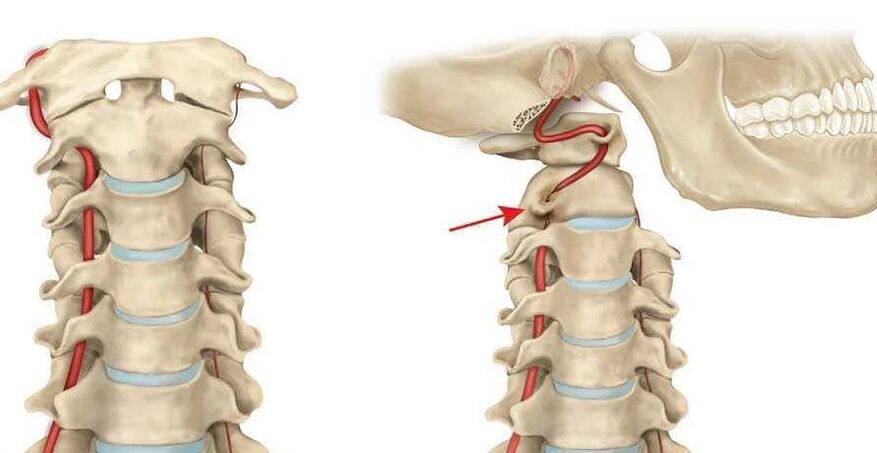
Vertebral artery syndrome
This syndrome is caused by a narrowing of the vertebral artery, which leads to vestibular, vascular and autonomic problems. In this case, the main symptoms are extensive:
- Headaches and migraines.
- Visual impairment.
- Ringing in the ears.
- Frequent dizziness and much more.
The most dangerous symptom is fainting, which indicates a severe lack of oxygen.
Radicular syndrome
It occurs when the roots of the spinal cord are damaged. In this case, nerve conduction is disrupted, a person may feel pain or lose sensitivity in certain parts of the body, or even suffer from paralysis.
Depending on which of the 8 radicular pairs the conduction disturbance occurs, the following symptoms are identified:
- 1 pair – numbness or pain in the back of the head;
- The third pair - impaired chewing reflex, numbness of the tongue and unpleasant sensations behind the ears;
- 4 pairs - pain in the collarbone area, impaired swallowing reflex;
- 5 pairs – disorders of the shoulder girdle, accompanied by problems with arm movement;
- 6th pair - the patient begins to feel pain and numbness in the forearm and shoulder blades;
- 7th pair - hands and fingers (usually index and middle) become numb;
- 8th pair – similar problems to the previous point, but numbness is felt in the ring finger and little finger.
Based on the features described, it is sometimes possible to determine which pair of roots is affected by radicular syndrome.
Cardiac syndrome
Despite the fact that the pathological process is still localized in the cervical spine, the syndrome has all the signs of cardiac pathologies. The clinical picture is as follows:
- Rapid pulse.
- Pain in the sternum.
- Shortness of breath, weakness, lethargy, decreased performance.
The rate of disease development
When we talk about the degree of osteochondrosis of the cervical spine, we mean the stages of progression of the pathological process, which differ in clinical signs. In total, there are four degrees of development of the disease:
- The first stage is characterized by vague symptoms. Patients complain of minor headaches; during the initial examination, the doctor notices a slight degree of muscle stiffness.
- Pain in the cervical spine and head is more common, more intense and radiates to the shoulder and arms. The pathology is caused by damage to the intervertebral discs and compressed nerve roots. The pain intensifies when you turn your head, throw it back and bend forward.
- In the third stage, the pain is constant, muscle weakness is observed in the arms and hernias are formed in the intervertebral discs. Movements in the neck area are limited, and frequent dizziness is present.
- The fourth stage is associated with complete destruction of the intervertebral disc, cartilage tissue is replaced by connective tissue. In addition to pain and dizziness, coordination problems are observed and the vertebral arteries are often compressed.
Signs and symptoms of cervical osteochondrosis
In order to consult a doctor at the right time, it is necessary to clearly understand the signs of cervical osteochondrosis. In some cases, such knowledge allows you to seek help in the initial stages of the disease, when it is easier to treat.
In general, the symptoms of osteochondrosis of the cervical spine are as follows:
- Pain in osteochondrosis is always present, only the intensity and frequency vary. Pain is the first clinical sign. Their intensity depends on the stage of disease progression, they are dull or compressive in nature. Painful sensations are present mainly in the neck and occipital region, but can also radiate to the temporal region, shoulder girdle and arms.
- In most cases, there are manifestations of damage to the vestibular apparatus. We are talking about frequent dizziness without cause, nausea, poor coordination of movements, uneven gait, loss of space.
- One of the most common clinical signs is stiffness of the neck muscles and stiffness of movement. It is difficult for a person to turn, sit down and turn his head back, the movements are accompanied by pain attacks.
- Many patients report a sensation of "goosebumps" running through the scalp or a characteristic tingling sensation.
- Muscle weakness and numbness occurs in the arm area.
- There are often psychological manifestations, expressed in depression, drowsiness, sudden mood changes, short temper or irritability.
- Due to poor circulation and damage to brain tissue, dizziness intensifies and noise in the ears appears, similar to rustling, pulsation and noise.
- Most patients notice deterioration of vision, as well as pain in the eyeballs, especially when trying to close the eyes too far to the left, right, up or down.
Sometimes it is possible to determine the degree of development of the pathological process from the symptoms. However, for a complete diagnosis this is still not enough and a number of diagnostic measures are required.

Diagnostic methods
The diagnosis of cervical osteochondrosis is necessary to determine the location and stage of disease progression. For a complete diagnosis, the following diagnostic methods are needed:
- Radiography is the main method for determining the degree and location of spinal deformity.
- Computed tomography can be used to more accurately diagnose pathological changes in vertebrae and intervertebral discs.
- MRI (magnetic resonance imaging) - enables detailed examination of discs and vertebrae, determination of the presence of hernias, protrusions, extent of lesions, etc.
- Dopplerography - with this examination, it becomes possible to find the place of compression of the artery and assess the degree of blood circulation disorders.
Treatment methods
Treatment of osteochondrosis of the neck always involves an integrated approach. The principles of treatment depend on a multitude of factors, such as the age of the patient, the stage of development of the disease, the severity of the clinical picture, etc.
However, in this situation you cannot do without a doctor and first of all you can contact a general practitioner, who will then refer you to a vertebrologist.
As for the integrated approach: osteochondrosis of the cervical spine is treated with the help of drug therapy, physiotherapy, massages, exercise therapy and other methods, which are worth talking about in more detail.
Drug treatment
The basis for the treatment of cervical osteochondrosis is drug therapy, which includes the use of tablets, drugs and medicines of the following groups:

- Painkillers - analgesic and antispasmodic. The former directly weaken the nerve centers, thus relieving painful sensations. The latter allow you to ease the spasm of the neck muscles, improving blood flow and suppressing pain.
- NSAIDs - non-steroidal anti-inflammatory drugs are necessary to reduce inflammation, most of them also eliminate pain. Often these medications are used in the form of gels or ointments that are rubbed into the affected area.
- Muscle relaxants are another way to relieve muscle spasms in the cervical region.
- Chondroprotectors are mandatory in certain stages of osteochondrosis of the spine, because they contribute to the restoration of bone tissue.
- B vitamins - normalize the metabolic processes of nervous tissue, improving the conduction of nerve impulses and promoting the functioning of the central nervous system.
Remember, the treatment should be carried out only under the supervision of a doctor, who is responsible for prescribing any medication, as well as determining the duration of use and its dosage.
Physiotherapy
Treatment of osteochondrosis of the neck will be many times more effective using certain physiotherapy techniques:
- Electrophoresis.
- Laser therapy.
- Ultrasound.
- Massage.
Massage therapy must be performed by an experienced medical professional, the treatment is carried out in a course of at least 10 sessions. Cervical massages help normalize blood circulation, restore elasticity, muscle tone, relieve pain, etc.
Physiotherapy
Therapeutic exercises also help speed up recovery, but are only performed during the recovery stages. It is important that the exercises do not cause discomfort or pain to the patient. Exercise therapy aims to strengthen muscles and relieve discomfort during movements by increasing the elasticity of muscle fibers.
The exercise technique is first developed by a physiotherapist, then the patient can independently perform gymnastics at home.
Manual therapy
Manual therapy is based on the principle of restoring motor functions and mobility between vertebrae. Initially, the manipulations consist of a light relaxing massage, then the doctor applies more and more force, exerting pressure and turning the neck to the vertebrae.
Applicator Kuznetsov
The use of Kuznetsov applicators is one of the methods of treating diseases of the spine, including osteochondrosis. The effect of the device on the cervical spine normalizes metabolic processes, relieves pain, increases muscle tone, improves blood circulation, increases the conductivity of nerve tissues, etc.
Treatment at home
The whole range of therapeutic measures is carried out at home, with the exception of physiotherapy, massages (in some cases) and the first stages of exercise therapy. However, now we are talking about traditional medicine and we will consider some of the most effective recipes:
- To use horseradish - take a leaf of this plant, pour boiling water over it and apply the inside to the neck, fixing it with a bandage. Can be left on while you sleep to enhance the effect.
- If there are no contraindications from a doctor, warming the cervical spine would be a good remedy. The easiest way is to use a pepper plaster, but you can heat the cake with wax, applying it 1-2 times until it cools completely.
Disease prevention
To prevent the development of the disease or its return after treatment, it is necessary to prevent osteochondrosis of the cervical spine. It consists of the following simple recommendations:
- Sleep on a flat and firm surface; it is better to buy a special orthopedic mattress and a pillow that takes the shape of the head.
- To prevent the disease, monitor your physical activity and do not overload the spine. If you have to lift weights, do it smoothly and keep your back straight.
- If your job requires you to sit for long periods of time, take breaks. Every hour you should walk or stretch your stiff muscles with simple gymnastic movements.
To prevent osteochondrosis, it is useful to swim and hang on the horizontal bar for 2-3 minutes every day.
























