In the structure of the pathology of the osteoarticular system, osteoarthritis occupies a leading place - about 70% of cases fall into its category. A similar problem is most often encountered by people after 50 years, but the initial signs of the disease appear even in young people. This disease has a serious medical and social importance, because in many cases it becomes the cause of functional failure in working age.
Many people know about a pathology such as arthrosis of the joints, but not every patient understands why it develops, how it manifests and what is required to fight the disease. And increased awareness and care can prevent harmful changes from occurring and progressing.
reason
Osteoarthritis is characterized by the development of degenerative-dystrophic processes in all joint tissues: cartilage, subchondral bone, ligaments, muscles and tendons. The disease is considered one of the "companions of aging", because it often affects elderly patients. But the age factor is far from the only cause of deforming arthrosis. The origin of the disease is quite heterogeneous and is due to external and internal types of pathological effects on the body.
For each patient, there are several risk factors that contribute to the appearance of joint pathology. Therefore, the causes of arthrosis combine the following conditions:
- Hard physical work.
- Inactivity.
- Traumatic injuries.
- Joint dysplasia.
- Inflammation (arthritis).
- Overweight.
- Estrogen deficiency in menopause.
- Diseases of the thyroid gland.
- Consequences of joint operations.
- Inheritance.
As you can see, the development of arthrosis is mediated by heterogeneous factors, which in most cases are of a mechanical or metabolic nature. In this case, the lifestyle of the patient and his profession are of no small importance, because loaders, manual workers and athletes often suffer from arthrosis.
The causes of arthrosis are quite different, they are characterized by a local effect on the joints and a general effect on the body.
Mechanism of development
The normal function of the joint is ensured by the harmonious work of all its structures. But the main component of any joint is cartilage. Provides shock absorbing function and resists pressure on joints. Cartilage tissue consists of cells (chondrocytes) and a matrix, the main substances of which are proteoglycans and collagen.
If the load on the joint exceeds the permissible, then first there are structural disorders in the cartilage. The proteoglycans that hold the collagen fibers are lost, which increases the tissue's sensitivity to external influences. The processes of destruction begin to prevail over synthesis. This is facilitated by a decrease in cartilage trophism when the synovial fluid contains an insufficient amount of nutrients. The imbalance of tissue renewal is supported by inflammatory reactions and hormonal disturbances.
All this leads to the thinning of the cartilage, it becomes rough and loses its elasticity. Due to the growth of the underlying bone tissue, the joint space narrows and osteophytes are formed - marginal growth. The synovial membrane thickens, ligaments thicken and shorten, and muscle function is impaired.
Pathological processes in the joints develop gradually, but do not pass without leaving a trace. Disorders in cartilage and other structures inevitably affect the clinical picture of osteoarthritis.
Distribution
Arthrosis, like other diseases, has certain varieties. This should be taken into account in the clinical classification of the disease. The pathology is primary when it develops in healthy joints, or secondary if it appears against the background of other diseases. In the case when the cause cannot be determined, they speak of idiopathic osteoarthritis. Depending on the number of nodes involved, the following varieties are distinguished:
- Monoarthrosis.
- Oligoarthrosis - no more than 2 joints are affected.
- Polyarthrosis - involving 3 joint groups.
If the pathological process has a generalized character, then we can talk about the loss of almost all joints of the body, including the spine, where spondylarthrosis is observed. In this case, the disease can continue in nodular or nodular form.
It is important to understand what processes occur in the joints and to adequately assess their severity. Therefore, be sure to consider the stage of arthrosis. It does not depend on the cause and is determined by pathological changes in the articular tissues:
- Stage 1 - inflammation of the synovial membrane, loss of the cartilage's ability to withstand the load.
- Stage 2 - destruction of cartilage tissue, bone growth, dystrophy of the joint bag.
- Stage 3 - bone deformation, contractures, joint instability.
The presence of signs of inflammation should also be reflected in the classification. Therefore, osteoarthritis is distinguished with and without synovitis. In addition, the functional state of the joint is important, which is determined by the degree of insufficiency:
- 1 degree - temporary limitation of function.
- Class 2 - disability.
- 3 degrees - the impossibility of self-service.
All these characteristics should be reflected in the diagnosis of osteoarthritis, as they are important for subsequent therapy.
Symptoms

Among articular pathology, the symptoms of arthrosis have a very tangible specificity. They develop gradually, but progress steadily, leading to a limitation in the patients' physical activity. Therefore, it is especially important to suspect the disease in time so that you can stop its development, as well as prevent complications.
When you contact a doctor, first of all, patient complaints are analyzed. And mostly people are worried about joint pain. But with arthrosis, unlike other pathologies, such as arthritis, they have the following character:
- Mechanical - occur against the background of load and decrease at rest.
- Onset - the appearance of pain is associated with the start of movement (walking).
- "Articular rat" - periodic sharp pains with joint blockage, caused by damage to the synovial membrane between the cartilaginous surfaces.
At first, patients may experience only vague discomfort in the joints, accompanied by a feeling of fatigue. But over time, it develops into pain. And if in the initial stages it bothers after a load, then in the future - during movement, and in advanced cases it becomes constant, remaining even at rest and at night.
In addition to pain, patients have other symptoms of arthrosis. They are both subjective and objective in nature, including the following characteristics:
- Stiffness in the joints in the morning no more than 30 minutes.
- Crackling sensation (crepitus) during movement.
- Deformation of the periarticular region.
- Restriction of mobility.
With arthrosis of the hands, during the examination, characteristic formations can be observed in the region of the proximal and distal phalanges - Bouchard's and Heberden's joints. The sensation of the affected joints is often painful. If contractures are formed, then there is a fixation of certain parts of the limbs more often in a flexion position.
The pronounced nature of osteoarthritis leads to a significant decrease in the level of physical activity of patients, which leads to a decrease in their quality of life.
Diagnosing
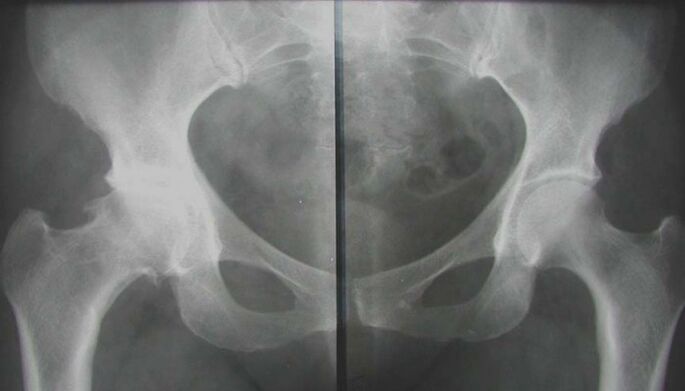
To understand why the clinical picture develops, it is necessary to confirm the pathology of the joints. This can be done by performing the necessary diagnostic examination, which includes instrumental and laboratory methods. First of all, they try to see structural changes in the affected areas, to assess their severity and prevalence. It is also necessary to determine the metabolic disorders in the body, which have become a favorable background for the appearance of arthrosis. Therefore, the survey complex consists of the following activities:
- Radiography.
- Magnetic resonance imaging.
- Ultrasound procedure.
- Arthroscopy.
- Biochemical blood tests (hormonal spectrum, markers of inflammation, calcium metabolism, rheumatic tests).
After the examination, a consultation with an orthopaedist-traumatologist will be required, who will help to form the correct treatment tactics for each patient.
Treatment

It is necessary to comprehensively treat joint arthrosis. This means that all available therapeutic agents are used to alleviate the patient's condition. But you should understand that their effectiveness directly depends on the treatment time. With advanced forms of the disease, conservative measures will help little. A pronounced and lasting result can be achieved with early treatment. For the treatment of osteoarthritis, the following methods are used:
- Medical therapy.
- Physiotherapy.
- Physiotherapy.
- Massage.
- The operation.
Which funds are suitable for a particular patient, the doctor decides. The choice is made based on the results of the examination and the individual characteristics of the organism.
The best treatment effect can be achieved if the correction begins in the early stages of the disease, when the first symptoms have just begun to appear.
General recommendations
Since the development of degenerative changes in the joint is mediated by an increased load, it is first necessary to reduce the mechanical effect on the cartilage tissue. To do this, you should stop wearing heavy and intense sports training. To unload the joint, any method is suitable - from walking with a cane to special fixation orthoses. But it is impossible to completely abandon movements, physical activity must be dosed. Walking short distances, swimming are useful.
Proper nutrition plays an important role in correcting arthritic changes. Diet helps to improve the condition of the cartilage, but it is also the main component of the fight against excess weight. Patients are advised to consume lean meat and poultry, fish, cereals; you should enrich the diet with fresh vegetables and fruits, herbs. But in return, you should refrain from smoked, spicy, fatty foods, marinades and pickles. It is better to pay attention to foods rich in collagen fibers, elastin and gelatin: jelly meat, hash, aspic dishes, fruit jelly.
Medical therapy

Traditional treatment of osteoarthritis begins with medication. Using various drugs, it is possible to eliminate not only the symptoms of the disease, but also to affect the mechanisms of its development. This is especially important in chronic degenerative joint pathology, when it is necessary to achieve a structure-modifying effect on cartilage tissue. The following medications are generally recommended:
- Non-steroidal anti-inflammatory.
- Chondroprotectors.
- Vascular.
- Vitamins and antioxidants.
- Metabolic (estrogens, thyroid hormones).
With severe pain in arthrosis, intra-articular injections of glucocorticosteroids can be made. But such treatment should be short-term, because with prolonged use, hormonal drugs have the opposite effect - they stimulate dystrophic processes. Systemic therapy should be combined with local drugs.
Taking medications for osteoarthritis is carried out with the doctor's recommendation and under his control. Independent use of any medicine is not allowed.
Physiotherapy
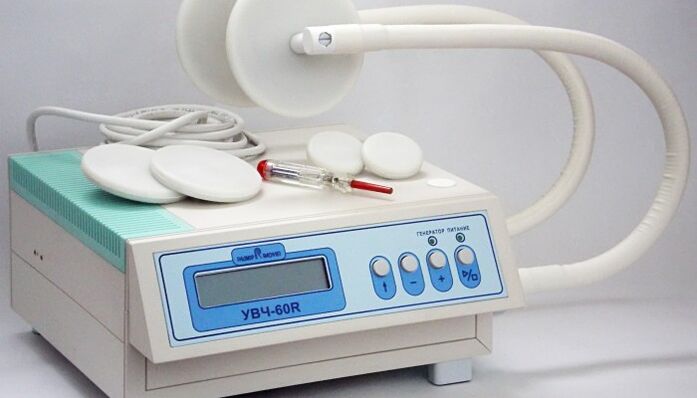
Methods of physical influence help to eliminate acute signs of joint pathology. Together with medications, they can reduce the severity of pain and inflammation, as well as stimulate biochemical processes in the cartilage itself. In the complex treatment of arthrosis, the following procedures are used:
- Electrophoresis.
- Ultrasound treatment.
- wave therapy.
- Magnetotherapy.
- laser treatment.
- Mud and hydrotherapy.
Such methods affect not only the joint, but also the surrounding tissues. This contributes to the activation of blood circulation, improvement of trophic processes and weakening of muscle contractures. Many elements of the spa treatment have a general health-improving effect. But at the same time, one should not forget about contraindications to physiotherapy: infectious diseases, tumors, cardiovascular pathology, kidney failure, bleeding, serious condition of the patient.
Physiotherapy
An important aspect of non-drug therapy for osteoarthritis is exercise therapy. It is known that the metabolism of cartilage tissue has a clear dependence on the mechanical factor. But his strength should be enough. Only then do processes of growth prevail over destruction. Therefore, gymnastics is indicated for all patients with joint diseases. But for each person, their own set of exercises is developed - taking into account the location and severity of the lesion, as well as the general condition of the body.
During classes, pain should not be allowed to appear. Exercises are performed at a slow pace and only after the acute symptoms have been eliminated. Avoid sudden and high-amplitude movements that can provoke discomfort. Physical education should be done under the supervision of a doctor and after you have acquired the necessary skills, you can start exercising at home.
Therapeutic gymnastics is an integral component of the correction of degenerative-dystrophic processes in the joints. Only regular classes have a positive result.
Massage

To improve the condition of the musculoskeletal system, massage sessions are indicated. Manual impact on joints allows you to achieve relaxation of spasmodic muscle groups, stimulate blood circulation in soft tissues and prepare them for active exercises (before therapeutic exercises). Classic massage includes the following elements:
- The caress.
- Trituration.
- Boiling.
- the pressure.
- Ironing.
It is often combined with passive movement in the affected joints. The duration of the therapy is determined by the doctor and can be from 7 to 15 sessions.
operation
If the advanced stages of osteoarthritis do not allow obtaining the desired effect from conservative measures, then there is a need for surgical treatment. Its essence is to replace the joint with an artificial one - arthroplasty. This operation is performed openly and under general anesthesia. After its completion, you must undergo rehabilitation, which begins as soon as possible. And as a result of the surgical intervention, the patient can completely get rid of arthrosis and return to an active life. True, the operation is not available to everyone.
Osteoarthritis is a common problem that requires a timely and active solution. In order not to start the disease and to be able to hope for the success of conservative measures, treatment should be started as soon as possible. This will avoid aggravations, prevent the progression of changes in the joints and restore the functional abilities of the musculoskeletal system as much as possible. Otherwise, surgical correction will have to be considered.
























